Top 10 Accounts Receivable AR Scenarios and How to Overcome Them? Professional Medical Billing Services
It serves as a measure of collection efficiency, and a lower number is often indicative of a more efficient medical billing process. The provider bills the patient’s insurance company for the services rendered, totaling $1,000. The insurance company processes the claim and reimburses the provider $800. The remaining $200 becomes part of the accounts receivable balance until it is collected from the insurance company. The RCM industry experts recommend healthcare organizations maintain their average days in accounts receivables to 35 days or less to ensure a steady cash flow and healthier revenue cycle. Accounts receivable in healthcare are the outstanding payment for the rendered care services owed to the healthcare practitioner by the patient or the insurance company.
- Proactive measures, robust training programs, and the use of technology can empower providers to overcome AR challenges and focus on delivering quality patient care.
- Healthcare organizations with effective AR management have seen denials below 5%.
- These cost calculations will play a primary role in establishing A/R thresholds.
- You can charge your patients upfront to avoid accounts receivable altogether.
- Medical providers can significantly boost their cash flow by submitting error-free claims.
Managing AR in Healthcare

Because of this hefty burden, healthcare providers collect on less than half of payments owed each year. Medical billing is directly linked to how quickly and accurately a healthcare provider receives payment. It covers claim creation, submission, and follow-up with insurance companies and patients. Any delay or error in this process can extend the time it takes to collect payments, increasing outstanding balances and weakening cash flow. Effective AR management is crucial for maintaining a healthy revenue cycle in healthcare.
Why it matters for healthcare and life sciences companies
With a strategic approach to AR management, healthcare organizations can ensure financial stability and long-term success. Until the healthcare provider receives payment from the payer, the amount owed for the services provided remains as part of https://eatagroup.com/2024/06/19/how-to-start-a-bookkeeping-business-in-7-simple/ their accounts receivable in healthcare. The healthcare provider records the expected reimbursement in their accounts receivable ledger, tracking the outstanding payment until it is received. AR Days is a vital metric for any healthcare provider, as it directly impacts the organization’s cash flow and financial stability. The longer it takes to collect payments, the more it strains your practice’s ability to cover operational costs and invest in growth. Identifying the major causes of claim denials is important for efficient accounts receivable management.
Nurture Patient Relationships and Inform Them About Financial Responsibilities
Did you know hospitals submitted around $3 trillion in claims, but $262 billion (9%) were initially denied? Better staff, resources, and care could have been provided with the money that was lost. Improves Creditworthiness Maintaining steady cash flow through AR financing can improve your ability to secure other financing if needed.
Help Patients Understand Their Payment Responsibilities
- Understanding and managing AR Days is essential for healthcare providers to maintain a steady cash flow and improve their revenue cycle.
- Whereas, Accounts Payable includes the outstanding bills that a hospital owes to another party.
- Also, your collection process needs to be revised to identify why are you slow in collecting your charges.
- Let’s look closer at some specific examples of how to employ AR in medical billing and other healthcare situations.
- Gathering patient information such as payment needs sets up both patient interactions and billing transactions for success moving forward.
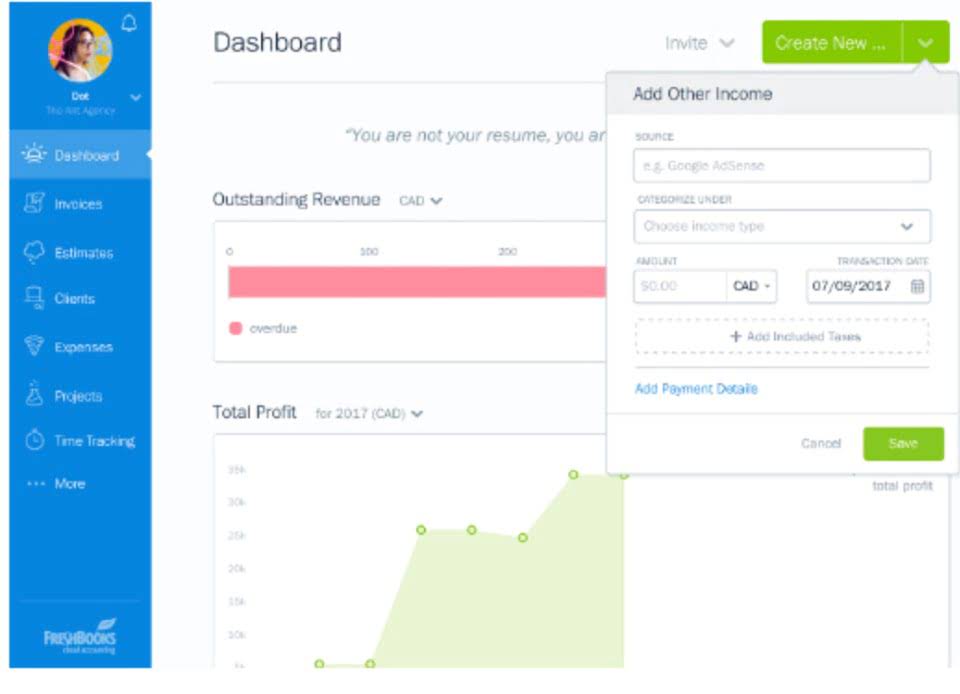
Reduces Dependence on Loans Provides an alternative to traditional loans or credit lines, often with simpler approval processes and flexible terms. Improves Cash Flow Stability Receives immediate funds for unpaid invoices, ensuring money is available for daily operations and emergencies. We are a dedicated team with the goal of providing our clients with an end-to-end solution that https://www.bookstime.com/articles/tax-season is 100% transparent throughout the process.


Besides, it is a financial metric that enables providers to oversee revenue streams for a steady cash flow. It defines the unreceived but recognized revenue and is recorded as a current asset in the statement of financial position. It constantly changes as providers perform new care services for patients while reimbursements, write-offs, and adjustments are made to the billing. QWay alleviates financial strain by promoting effective management and improved economic outcomes for healthcare providers. In medical billing, the HCFA 1500 form or the CMS-1500 form is one of the important forms.
Ensure Regulatory Compliance
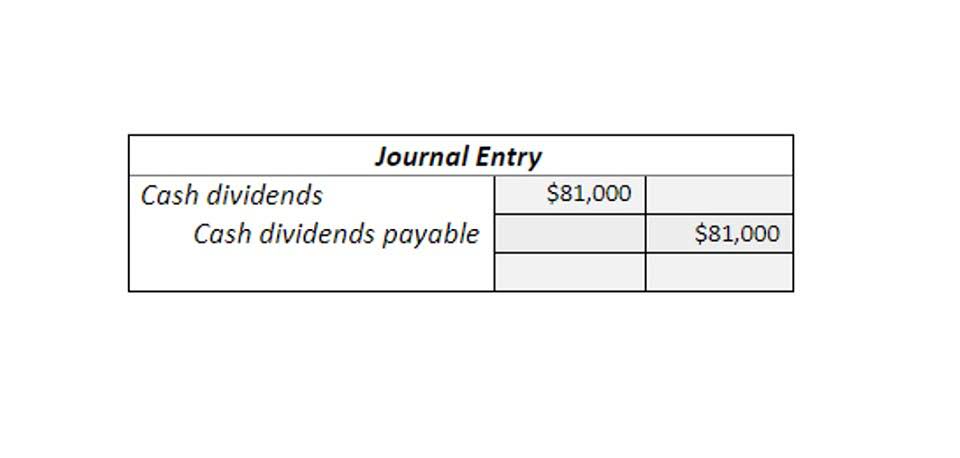
The graph below shows the contrast between Better-performing billing departments vs. accounts receivable in healthcare Average-performing billing departments. For a long time if the account goes uncollected then the provider suffers not only loss of revenue but needed to set aside resources for collection. 86 days look excessive due to payer mix or some circumstance of a major payer. Also, your collection process needs to be revised to identify why are you slow in collecting your charges. Analyzing and optimizing A/R reports in health care is critical to making a strong financial structure for your practice. Healthcare providers must take a proactive stance to preserve a sustainable AR process.

Accounts Receivable in Medical Billing
The first stage ( pre-invoicing) includes setting up the patient or payer accounts, establishing payment terms, and confirming the creditworthiness of the patient. The pre-invoice step sets the foundation of the entire healthcare AR process. During this stage, accounts receivable companies help you to conduct a patient’s credit check, establish payment terms, and set up the patient account efficiently.
